QUICK FACTS
Milestone: First person infected with SARS
Date: Nov. 16, 2002
Where: Foshan, China
Who: A food handler
In January 2003, epidemiologists in China identified two cases of “atypical pneumonia” in patients who had visited health care workers in Guangdong province. Teams initiated contact tracing and eventually discovered that the germ responsible for the illnesses had been circulating since a patient fell ill Nov. 16, 2002.
Those early cases in November were in “food handlers” — those who either worked as chefs in restaurants or as vendors at “wet markets,” where live animals, such as poultry and more-exotic animals like civet cats and raccoon dogs, were held in crowded conditions.
By the time Chinese disease investigators realized an outbreak might be unfolding, the disease had already been circulating for two months and had spread to health care workers.
The disease reached Hong Kong in February and then exploded when a nephrologist from southern China traveled to the region for a wedding on Feb. 21, 2003. He was unwell during his trip and later died of the disease.
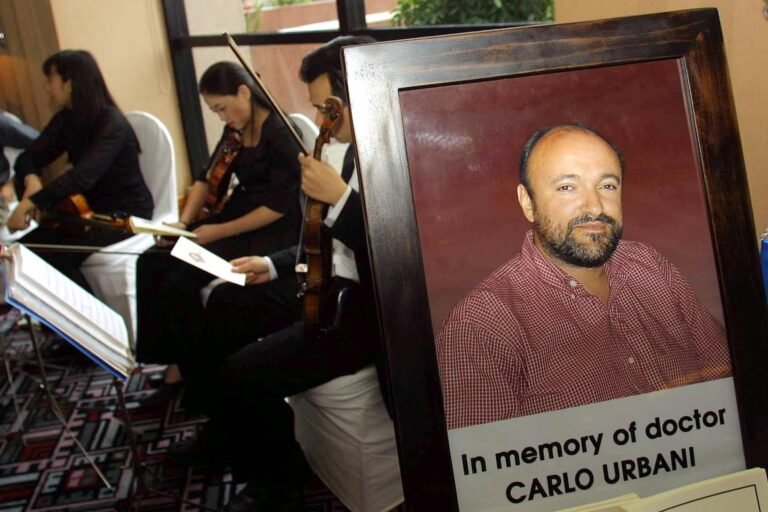
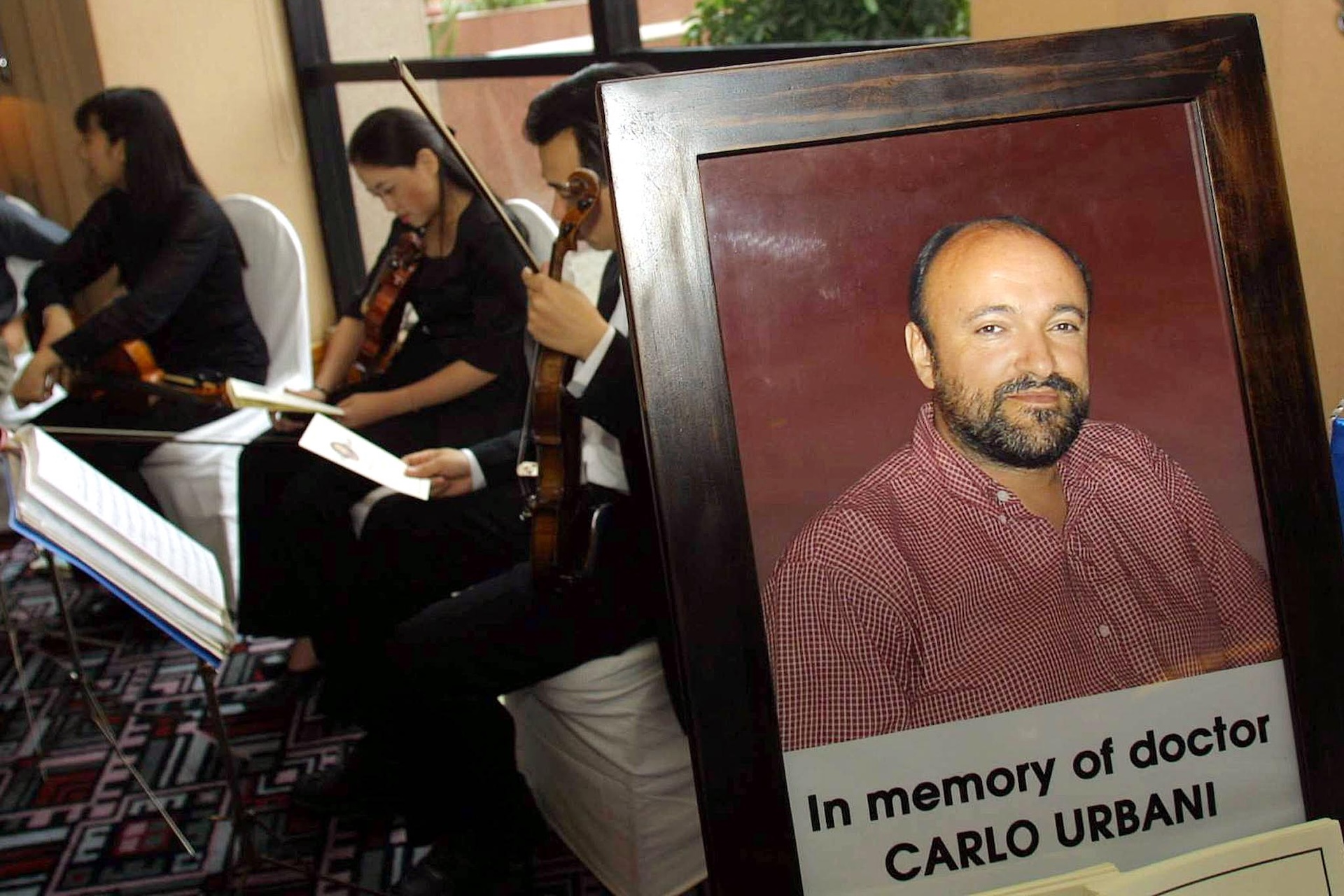
In March, a case investigator for the World Health Organization (WHO), Dr. Carlo Urbani, came to investigate a case observed in a businessman who had traveled to Hong Kong before arriving in Hanoi, Vietnam, and being hospitalized there. Urbani ultimately acquired the disease himself and died that same month.
By March 12, the WHO had issued an alert about a severe form of pneumonia of unknown origin in people from China, Hong Kong and Vietnam. By March 15, the Centers for Disease Control and Prevention (CDC) had officially named the disease severe acute respiratory syndrome (SARS), and by March 24, they had identified a novel coronavirus as the cause.
By that time, the outbreak had neared its peak. The pandemic lasted for months, spread to 28 countries beyond China —with 29 cases in the U.S. — and affected more than 8,000 people, 774 of whom died. The disease’s case-fatality rate was estimated to be around 9.6%.
In early 2004, SARS briefly flared up again, but its spread was quickly squelched through an aggressive and rapid contact-tracing-and-containment strategy.
That second flare-up enabled scientists to trace the SARS virus to palm civets and raccoon dogs sold at markets. The next year, scientists proposed that horseshoe bats were the pathogen’s original animal host, but it wasn’t until 2017 that researchers found the smoking gun: bats carrying a rich pool of SARS-like viruses living in remote caves in China’s Yunnan province. The caves were just a mile away from villages.
“The risk of spillover into people and emergence of a disease similar to SARS is possible,” authors warned in their paper at the time.
The SARS epidemic, as scary as it was at the time, was ultimately just a dress rehearsal for the COVID-19 pandemic that swept across the globe from March 2020 to May 2023, after early cases started to emerge in November 2019. The two viruses belong to the same general family of coronaviruses and likely emerged from a similar animal host.
Scientists and public health officials successfully applied some of the lessons of SARS to the COVID pandemic. For instance, when SARS first emerged, China had a very rudimentary infectious-disease surveillance system. While they did report cases of infectious and food-borne diseases, communication was by telephone call, there was no standardized case reporting system, and they had no system in place to track contacts or collect lab results. After the SARS epidemic, China quickly implemented a thorough contact-tracing and disease-surveillance system.

That would prove crucial when SARS-CoV-2, the coronavirus that causes COVID-19, emerged in China. The country logged hundreds of thousands of cases of infections during the first wave, which ended in China by mid-February — just a few months after investigators first reported a cluster of pneumonia cases of unknown cause in Wuhan. (A draconian lockdown also likely helped contain the virus’s spread within the country.)
Whereas it took months to identify the cause of the SARS pandemic, the SARS-CoV-2 virus was identified less than two weeks after the first cases were noticed. And SARS had no specific treatment, whereas by mid-March 2020, vaccines against the newly identified virus were in clinical trials, thanks to mRNA technology that had been in the works for decades.
Other lessons the world could have taken from SARS were only partially learned. In 2017, when the SARS source was identified, Dr. Kwok-Yung Yuen, a virologist at the University of Hong Kong who co-discovered the virus, told Nature News that the finding “reinforces the notion that we should not disturb wildlife habitats and never put wild animals into markets.” He told Nature News that respecting nature “is the way to stay away from the harm of emerging infections.” Yet the practice continued.
In some ways, the SARS epidemic also gave public health agencies a false sense of security. SARS and related coronavirus diseases, such as Middle East respiratory syndrome (MERS), were much deadlier than SARS-CoV-2 but also much easier to contain. Outbreaks were relatively easy to control using contact tracing and other public health measures, rather than requiring the distribution of vaccines.
That’s because SARS had a shorter infectious window than COVID-19. It was most infectious during the second week of the illness, when people were seriously ill, whereas SARS-CoV-2 was easily transmitted from the early phases of disease, sometimes even before symptoms emerged.